Calcific Tendinitis of the Shoulder
What is Calcific Tendonitis of the Shoulder (Calcifications)?
What is Calcific Tendonitis of the Shoulder (Calcifications)?
Calcific tendinitis or tendinopathy of the shoulder is an inflammation of the rotator cuff tendons caused by intratendinous deposition of calcium phosphate crystals (calcification). It is an important cause of shoulder pain and dysfunction that generally affects a young population of working age and is more common in women. Calcifications are not associated with trauma or previous accidents.
Up to 22% of the general population has calcifications in the rotator cuff tendons, but fortunately, in most cases the calcifications are asymptomatic. The supraspinatus tendon is the most affected and the probability of concomitant contralateral calcification is 14%.

What causes Calcific Tendinitis of the Shoulder?
What causes Calcific Tendinitis of the Shoulder?
The pathogenic mechanism that causes calcifications of the rotator cuff tendons is not yet well understood, but it is related to degenerative changes in the tendons and metaplasia of their cells, which begin to produce and deposit calcium deposits in the tendon itself.
There is an association between calcific tendonitis and other diseases such as:
- Diabetes
- Hypertension
- Ischemic Heart Disease
- Thyroid dysfunction
- Endocrine diseases
- There also appears to be a genetic and familial predisposition
- A sedentary lifestyle also increases the risk of this pathology.
Signs and Symptoms of Calcific Tendinitis of the Shoulder
Signs and Symptoms of Calcific Tendinitis of the Shoulder
The formation of calcium deposits is usually a slow process over several months and may cause mild pain or only minor discomfort. However, the pain may appear more suddenly and intensely during the period in which the calcifications are being reabsorbed. The pain is often described as radiating to the elbow and neck.
According to the natural history of the disease, we can divide the presentation of calcifying tendonitis into 2 large groups – Acute presentation: the pain is more intense and often associated with decreased shoulder mobility. It lasts between 2 and 3 weeks, or in some cases even a little longer. It is generally very disabling and it quite commonly affects sleep. Chronic presentation: the pain is not as intense as in acute cases and there may be periods when patients are asymptomatic. However, symptoms can last for several months.
Less frequently, calcific tendonitis can present as a frozen shoulder or adhesive capsulitis – Adhesive capsulitis: the pain is usually not so intense but there is a clear loss of mobility in the shoulder that will require long periods of rehabilitation
Diagnosis of Calcific Tendinitis of the Shoulder
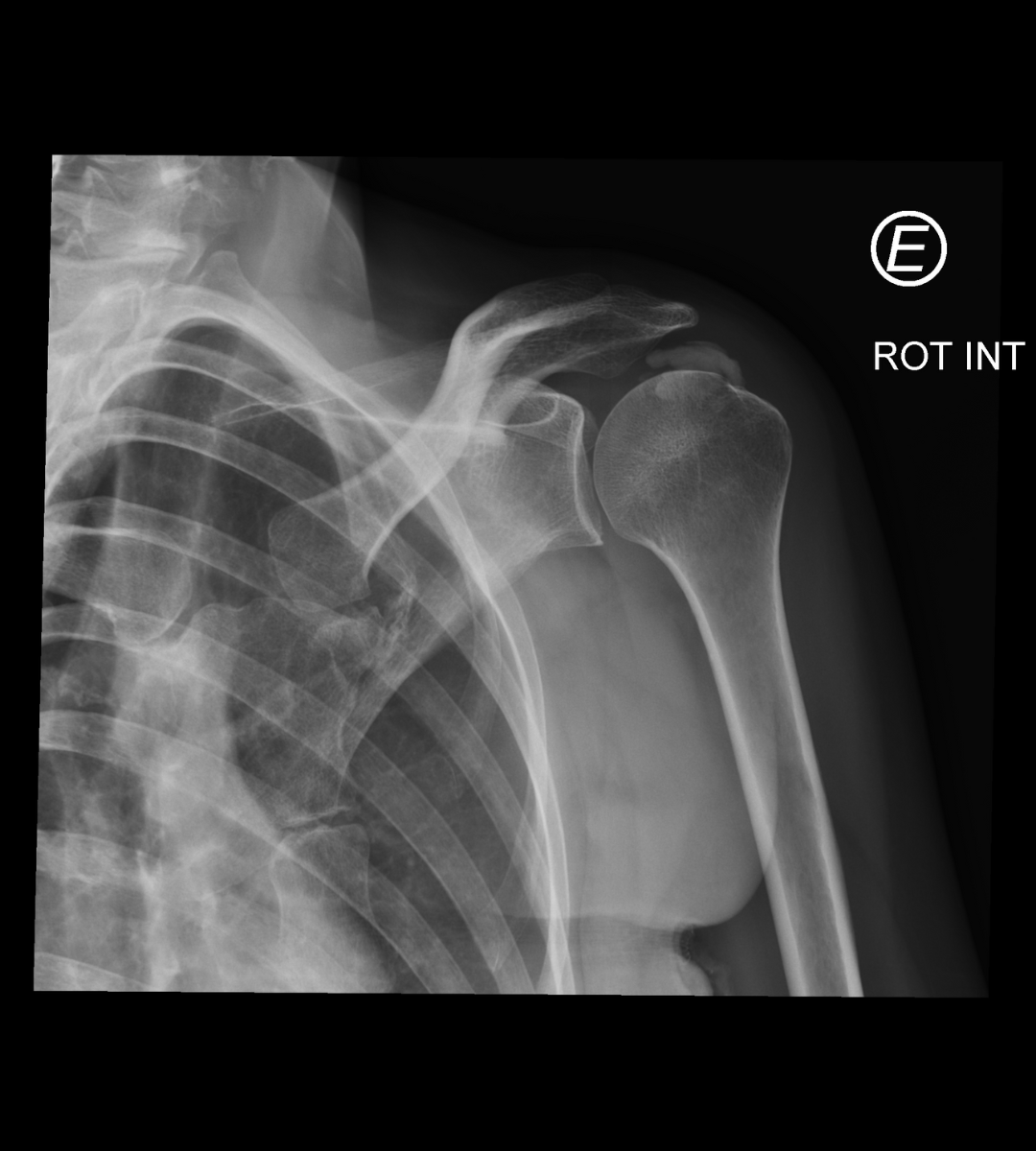
X-ray
This is often sufficient for the diagnosis of calcific tendonitis since the calcification is radiopaque and visible on radiographs.
Ultrasound
It allows microcalcifications to be observed that are often not visible on X-rays. The resolution of ultrasound is superior to that of magnetic resonance imaging for identifying calcifications. In addition, it is a dynamic examination that allows the presence of subacromial conflict to be observed.
Magnetic Resonance Imaging
It is a good complementary study that, in addition to allowing the diagnosis of calcifications, allows the evaluation and diagnosis of other shoulder injuries such as rotator cuff tears, labrum injuries and/or injuries to the long portion of the biceps, among others.
Treatment for Calcific Tendinitis of the Shoulder
Conservative
When to perform it? It is the first treatment method because, in most cases, the pain and other symptoms are self-limiting and the natural history of the disease shows us that in general the pain improves over time without the need for aggressive interventions. Treatment should be carried out in stages, always from the simplest to the most complex and always integrated into an individualized plan for each patient.
Treatment options?
- Medication and Rest: in the most intense phase of pain, it is essential to treat the pain. In this sense, the use of non-steroidal anti-inflammatory drugs and other oral analgesics is essential. In cases where pain control with oral medication is not sufficient, the use of corticosteroids may be considered, especially in patients whose sleep is significantly disturbed by the disease. Rest is essential in the initial phase to reduce pain, but should be self-limited over time. The shoulder is the most mobile joint in the human body and, therefore, as symptoms improve, it is essential to begin mobilizing the shoulder to prevent stiffness and muscle atrophy.
- Physiotherapy and Rehabilitation: a physical rehabilitation program can be essential in the recovery from this pathology, especially in cases where the clinical presentation is more prolonged over time. In these cases, it is common to observe changes in the normal movement of the shoulder or a decrease in shoulder mobility associated with changes in the position and normal kinetics of the shoulder blade, which can lead to subacromial conflict and perpetuate pain. Mobility exercises and exercises to improve the kinetics of the shoulder blade allow the shoulder to recover its homeostasis after these periods of active disease.
- Shoulder Infiltration with Corticosteroids: This may be necessary in patients with acute and intense pain associated with the inability to sleep, when oral medication is not sufficient to control the pain. It is an invasive procedure whose objective is to reduce pain and not to cure the disease.
- Shoulder Infiltration with PRPs: PRPs or platelet-rich plasma are growth factors that can help heal the inflammatory process and regenerate the degenerated tendon. This technique involves using the patient's own plasma and platelets, which are previously extracted and then undergo a centrifugation process to prepare these growth factors for later infiltration into the injured area. This procedure is performed on an outpatient basis and the patient is discharged immediately after the infiltration, if clinically stable.
- Shock waves: a non-invasive procedure that, similar to what is already performed in the treatment of kidney stones, breaks up calcium deposits and helps the body to reabsorb them. In general, several sessions (minimum 3) separated by 1 week each are necessary to reduce symptoms. This procedure should not be performed in isolation, but rather integrated into an individualized plan for each patient.
- Barbotage: minimally invasive procedure, guided by ultrasound, which allows the calcification to be located, fragmented and aspirated using a needle.
Surgical
When to perform? Mainly in chronic patients who do not respond to conservative treatment.
Technique Arthroscopic excision of calcification: minimally invasive procedure (incisions < 0.5 cm) that allows observation of the entire shoulder joint and drainage, aspiration of calcification and cleaning of inflammatory tissues from the shoulder
Postoperative
- The arm is not immobilized
- Remove stitches at 2 weeks
- Physiatric rehabilitation for a period of 4 to 6 months
How to prevent Calcific Tendinitis of the Shoulder?
A healthy lifestyle with regular physical exercise is the only known way that can help prevent this disease, as it allows the maintenance of balance and stability of the shoulder.
When to seek an Orthopedic Specialist?
- Pain requiring analgesic medication for more than 3 days in a row
- Pain for more than a week, without the need for medication
- Pain associated with loss of mobility
- Nighttime pain that interferes with sleep
- If there was previous trauma
- Intense pain
Diagnosis of Calcific Tendinitis of the Shoulder
X-ray
This is often sufficient for the diagnosis of calcific tendonitis since the calcification is radiopaque and visible on radiographs.
Ultrasound
It allows microcalcifications to be observed that are often not visible on X-rays. The resolution of ultrasound is superior to that of magnetic resonance imaging for identifying calcifications. In addition, it is a dynamic examination that allows the presence of subacromial conflict to be observed.
Magnetic Resonance Imaging
It is a good complementary study that, in addition to allowing the diagnosis of calcifications, allows the evaluation and diagnosis of other shoulder injuries such as rotator cuff tears, labrum injuries and/or injuries to the long portion of the biceps, among others.
Treatment for Calcific Tendinitis of the Shoulder
Conservative
When to perform it? It is the first treatment method because, in most cases, the pain and other symptoms are self-limiting and the natural history of the disease shows us that in general the pain improves over time without the need for aggressive interventions. Treatment should be carried out in stages, always from the simplest to the most complex and always integrated into an individualized plan for each patient.
Treatment options?
- Medication and Rest: in the most intense phase of pain, it is essential to treat the pain. In this sense, the use of non-steroidal anti-inflammatory drugs and other oral analgesics is essential. In cases where pain control with oral medication is not sufficient, the use of corticosteroids may be considered, especially in patients whose sleep is significantly disturbed by the disease. Rest is essential in the initial phase to reduce pain, but should be self-limited over time. The shoulder is the most mobile joint in the human body and, therefore, as symptoms improve, it is essential to begin mobilizing the shoulder to prevent stiffness and muscle atrophy.
- Physiotherapy and Rehabilitation: a physical rehabilitation program can be essential in the recovery from this pathology, especially in cases where the clinical presentation is more prolonged over time. In these cases, it is common to observe changes in the normal movement of the shoulder or a decrease in shoulder mobility associated with changes in the position and normal kinetics of the shoulder blade, which can lead to subacromial conflict and perpetuate pain. Mobility exercises and exercises to improve the kinetics of the shoulder blade allow the shoulder to recover its homeostasis after these periods of active disease.
- Shoulder Infiltration with Corticosteroids: This may be necessary in patients with acute and intense pain associated with the inability to sleep, when oral medication is not sufficient to control the pain. It is an invasive procedure whose objective is to reduce pain and not to cure the disease.
- Shoulder Infiltration with PRPs: PRPs or platelet-rich plasma are growth factors that can help heal the inflammatory process and regenerate the degenerated tendon. This technique involves using the patient's own plasma and platelets, which are previously extracted and then undergo a centrifugation process to prepare these growth factors for later infiltration into the injured area. This procedure is performed on an outpatient basis and the patient is discharged immediately after the infiltration, if clinically stable.
- Shock waves: a non-invasive procedure that, similar to what is already performed in the treatment of kidney stones, breaks up calcium deposits and helps the body to reabsorb them. In general, several sessions (minimum 3) separated by 1 week each are necessary to reduce symptoms. This procedure should not be performed in isolation, but rather integrated into an individualized plan for each patient.
- Barbotage: minimally invasive procedure, guided by ultrasound, which allows the calcification to be located, fragmented and aspirated using a needle.
Surgical
When to perform? Mainly in chronic patients who do not respond to conservative treatment.
Technique Arthroscopic excision of calcification: minimally invasive procedure (incisions < 0.5 cm) that allows observation of the entire shoulder joint and drainage, aspiration of calcification and cleaning of inflammatory tissues from the shoulder
Postoperative
- The arm is not immobilized
- Remove stitches at 2 weeks
- Physiatric rehabilitation for a period of 4 to 6 months
How to prevent Calcific Tendinitis of the Shoulder?
A healthy lifestyle with regular physical exercise is the only known way that can help prevent this disease, as it allows the maintenance of balance and stability of the shoulder.
When to seek an Orthopedic Specialist?
- Pain requiring analgesic medication for more than 3 days in a row
- Pain for more than a week, without the need for medication
- Pain associated with loss of mobility
- Nighttime pain that interferes with sleep
- If there was previous trauma
- Intense pain